CMS is temporarily removing CPT codes 63685 and 63688 from the list of OPD services that require prior authorization. There may be occasions when a beneficiary requires services beyond those ordinarily covered by Medicaid or needs a service that requires prior authorization PA.
Http Covenanthealthcare Com Uploads Public Documents Workfiles Insurance Forms Precertification 20radiology 20guide 202018 Pdf
If you continue using one of these drugs without prior approval for medical necessity you may be required to pay the full cost.

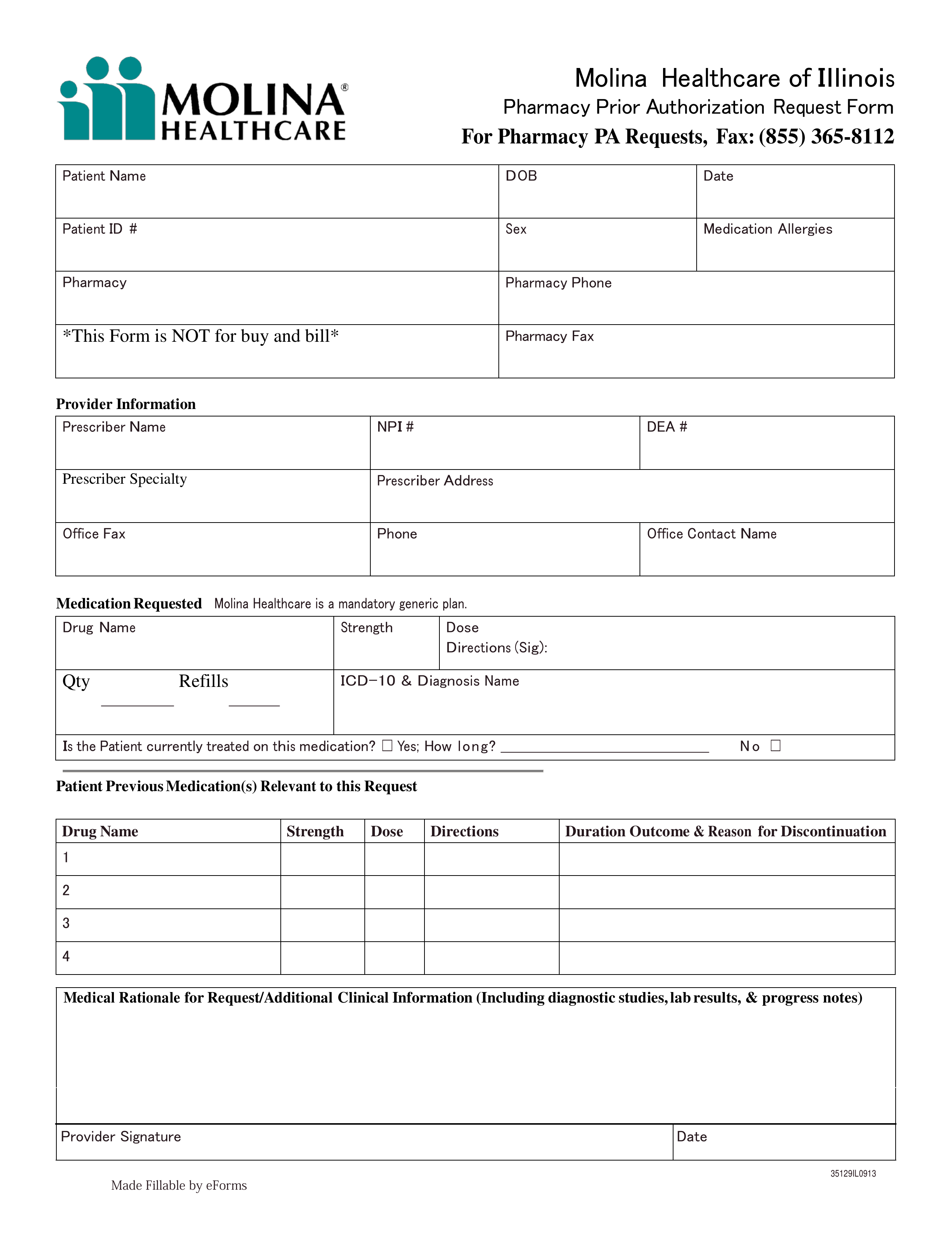
Prior authorization cheat sheet. Program Prior AuthorizationMedical Necessity Medication Humira adalimumab P. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure. Requesting Re-Authorization ExtensionsContinuing Care Re-Authorization requested by the provider before the End date of the previous PA or before units approved on previous PA are consumed prior to End date of previous PA.
Systemic Estrogen Prior Authorization Form for Medicare SuboxoneSubutex Prior Authorization Form for Commercial and Medicare Plans Fax completed Prior Authorization forms to Presbyterian Pharmacy Services at 505 923-5540 or at 1-800-724-6953. 122020 Clarified medically necessary language in the background. Prior authorization is one example of a range of evidence-based medical management.
102020 Removed coverage for triglycerides 500. When you create a TDY authorization in DTS the system accesses database information. Prior Authorization PA Inquiry Information Sheet 2019 Page 5 Updated.
Prior authorization requests usually require information that proves medical necessity such as. Humira adalimumab is indicated for reducing signs and symptoms inducing major clinical. CMS-1500 Claim Form Cheat Sheet.
23 - Prior Authorization number Where this populates from. December 6 2019 After reviewing each detail on the Details screen click Next and the Summary screen will be displayed. PA09 - Botulinum Toxins.
CMS-1500 Claim Form Cheat Sheet. NYS MEDICAID PROGRAM- ENTERAL FORMULA PRIOR AUTHORIZATION PRESCRIBER WORKSHEET To facilitate the process be prepared to answer these questions when you call the interactive voice response IVR Enteral Prior Authorization Call Line at 1-866-211-1736 Option 1. PA05 - Follicle Stimulation.
The following service categories comprise the list. Medicare Part A FaxMail Cover Sheet. PA10 - Agents Treating Pulmonary Hypertension.
See additional instructions and FAQ tips on reverse side. However this medication requires something called prior authorization typically used for prescription drugs. Medications Requiring Prior Authorization for Medical Necessity Below is a list of medicines by drug class that will not be covered without a prior authorization for medical necessity.
Prior Authorization PA Cheat Sheet. Or mail to the applicable addressnumber provided at the bottom of the page. Written by Sydney Updated over a week ago.
Providers who plan to perform both the trial and permanent implantation procedures using CPT code 63650 in the OPD will only require prior. 2021 Final List of Outpatient Department Services That Require Prior Authorization. PA06 - Growth Hormone.
PA04 - Weight Loss. PA02 - CNS Stimulants. Essentially the authorization is a means of informing everyone who needs to know when you will be gone where you will be working and how much you expect your trip to cost.
Prior Authorization for Non-Preferred Drug Form. The patients past medical history ormedical records Conditions symptoms and. The following is the list of codes associated with the list of hospital outpatient department services contained in 42 CFR 41983a1 and 2.
Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. This screen displays the summary of the authorization. A Mini Health Insurance Cheat Sheet.
Attach supporting medical documentation and fax to. ONE 1 Medicare Fax Mail Cover Sheet for each prior authorization request for which documentation is being submitted. Prior authorization is a process whereby a provider on behalf of a patient requests approval or authorization from the health plan before delivering a treatment or service in order for the treatment or service to be covered by the health plan.
For Medicaid to reimburse the provider in this situation MDHHS requires that the provider obtain authorization for these services before the service is rendered. Amount of time before the End date of the previous PA for provider to request a Re-Auth will be specified in the. Pharmacy Prior Authorization Program.
The only service that will require prior authorization for implanted spinal neurostimulators is CPT code 63650. Program Prior AuthorizationMedical Necessity - Vascepa icosapent ethyl Change Control Date Change 22020 New program. No matter what health plan you have you will see the terms providers in-network and out-of-network pop up.
In this guide you are the traveler unless stated otherwise. Patient File Insurance tab Prior authorization turned on Authorization Description.