Buckeye earned the top five-star rating for Keeping Kids Healthy and Doctors Communication and Service. We researched the best Medicare Part D providers based on.
 A Guide To The Nightmare Of Getting Health Insurance In A Pandemic The American Prospect
A Guide To The Nightmare Of Getting Health Insurance In A Pandemic The American Prospect
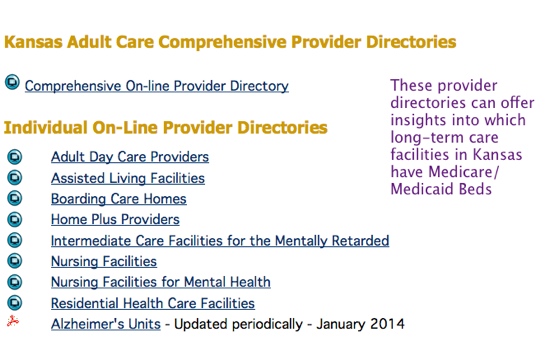
Provides Medicaid covered.
Best medicaid plan. The program has three parts. To learn more go to NC Medicaid Direct services. We can help.
Kaiser Foundation Health Plan of the Mid-Atlantic States Maryland. They all cover primary care medications hospital stays emergency care transportation to appointments and more. All of the Healthy Louisiana Medicaid health plans have the same core benefits.
Compare plans to see all Extra Services. Wwwmedicaidohiogov Call the Ohio Medicaid Consumer Hotline toll-free. HMO 45 4.
Managed Medical Assistance MMA. In Marylands HealthChoice program health care services are provided through managed health care organizations called MCOs. Read Review Compare Quotes.
Call us to get answers to your questions about NC Medicaid Managed Care. Use the chart to help pick your MCO. We focus on the whole person - their physical behavioral and social needs.
1-833-870-5588 Hours of operation. Available 24 hours a day 7 days a week. To 8 pm Monday through Sunday Or use the chat tool to chat with us online.
However you might be restricted as to which medical providers you can see. We provide access to quality care for people with complex needs. Plan C covers part B deductibles but not excess charge which could make it a good choice for those who want decent coverage without the higher premiums of plan F.
Ask your doctors which MCOs they accept or use the MCO provider search tool. NC Medicaid Managed Care restart. In 2019 NCQA rated more than 1000 health insurance plans based on clinical quality member satisfaction and NCQA Accreditation Survey.
In Florida most Medicaid recipients are enrolled in the Statewide Medicaid Managed Care program. The Ohio Department of Medicaid ODM awarded Buckeye Health Plan the highest quality rating among all Ohio managed care plans with 20 stars across the five categories on its 2018 Managed Care Plans Report Card published today. Jai Medical Systems Managed Care Organization Maryland.
Click a plan name for a detailed analysis. For answers to common questions go to Get answers. With wide availability and 247 on-call nursing services Aetna is one of the best Medicare Advantage providers for individualized plan solutions.
If you do not pick an MCO within 28 days you will be automatically assigned to one. AM Best gives Cigna an A for financial strength. HMO 50 2.
In addition a small group of people will be able to choose if they want to participate in NC Medicaid Direct or NC Medicaid Managed Care. Visit the Ohio Department of Medicaid online. To view health plans.
People on Medicaid will get services using one or more of these plan types. Which Medicare Part D Drug Plan offers the best prescription medication coverage for your needs. 1-800-324-8680 or go online.
NC Medicaid Direct is a way to get your Medicaid benefits if you cannot enroll in a health plan through NC Medicaid Managed Care. HMO 50 3. 5 Cigna offers a wide variety of Medicare Advantage plans including three types of Special Needs Plans for.
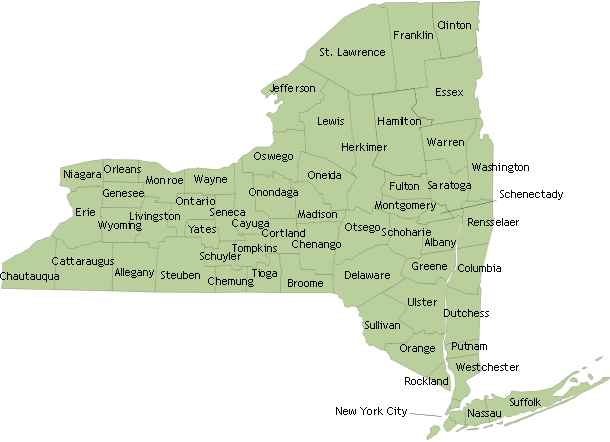
Capital District Physicians Health Plan New York. The call is toll free. Health Plans and Program.
619 million Americans are Medicare beneficiaries. Managed Medical Assistance Long-Term Care and Dental. 1 In 2019 more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs.
NCQA Health Insurance Plan Ratings 2019-2020 - Summary Report Medicaid Search for a health insurance plan by state plan name or plan type private Medicaid Medicare. Allways Health Partners Massachusetts. 15 best-rated Medicaid plans for 2019 1.
But there are differences in extra benefits like hearing. If you are Medicare dual eligible you may qualify for a Medicare D-SNP Dual Special Needs Plan which is a type of Medicare Advantage plan.