Prior authorization through the. Because this procedure is covered by Medicare it is more readily available to patients.
 Vertiflex Procedure Lumbar Spinal Stenosis Treatment Pain Com
Vertiflex Procedure Lumbar Spinal Stenosis Treatment Pain Com
The Vertiflex Superion device has been proven to last up to 2 years.

Is vertiflex covered by insurance. In fact over 25000 Vertiflex procedures have been performed. The success of using this small implant is revolutionizing the way spinal stenosis is being treated. How much is a SUPERION INDIRECT DECOMPRESSION SYSTEM.
Francis Magee DVM chief technology officer at Paradigm Spine told OTW Commercial payors are recognizing the value of coflex as part of the lumbar spinal stenosis treatment continuum. How long does Vertiflex last. When expanded the device relieves the compression on.
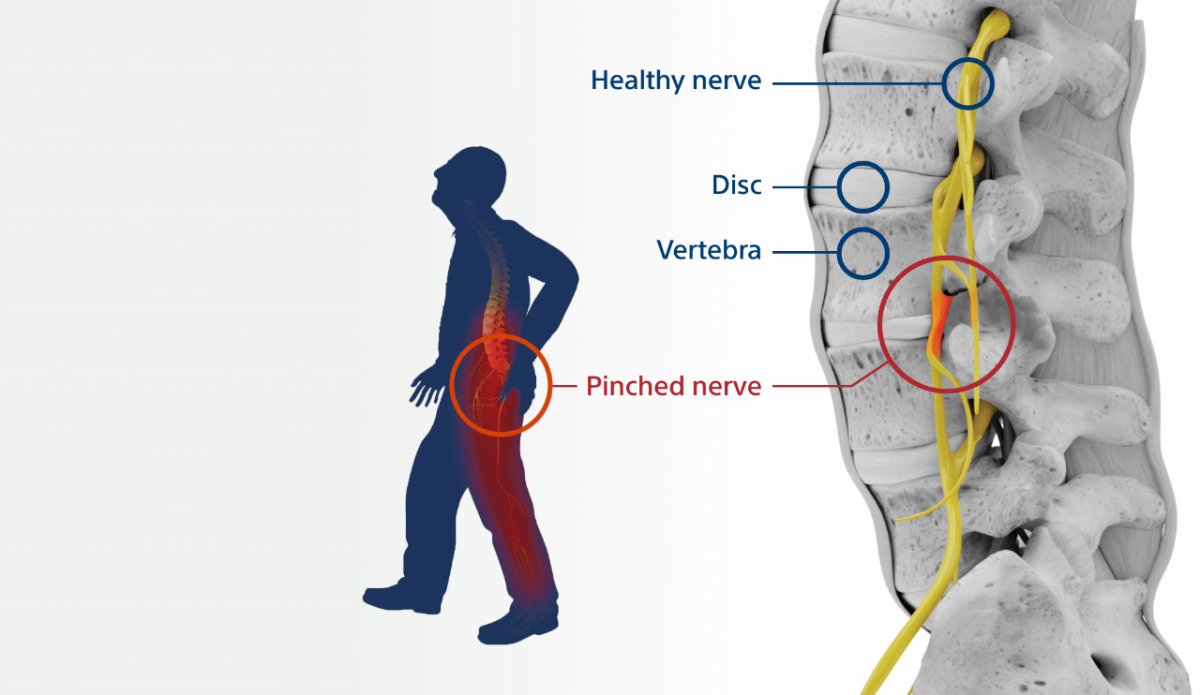
Nonsurgical treatment for LSS includes NSAIDs physical therapy andor epidural steroid injections. Despite the lack of coverage for PILD procedures patients enrolled in the approved CED clinical study for VertiFlexs Totalis Direct Decompression System will be able to receive Medicare coverage for the procedure. Call your insurance company to know if Vertiflex is covered in your insurance plan.
A SUPERION INDIRECT DECOMPRESSION SYSTEM COST on AVERAGE 12100 During this procedure your doctor will implant the superion device a small expandable spacer through a small incision in the lower back into the affected area of the spinal canal. The minimally invasive Vertiflex Procedure is FDA approved and backed by a long-term clinical study. The following are the 2020 Medicare coding and national payment rates for Interspinous Spacer procedures performed in the outpatient hospital setting.
Vertiflex is covered by Medicare Medicaid. LSS may be due to a bulging disk andor hypertrophy of the ligamentum flavum. 2020 Quick Reference Guide The Vertiflex Procedure Outpatient Hospital2020.
Is Vertiflex covered by insurance. Percutaneous Interspinous Spacer VertiFlex MP9544. VertiFlex is a privately held medical device company dedicated to the advancement of minimally invasive solutions for the treatment of lumbar spinal.
SAN CLEMENTE CA January 14 2014 VertiFlex Inc a leading innovator of advanced minimally invasive spinal surgery technologies announces The Centers for Medicare Medicaid Services CMS has released its final Decision Memorandum on coverage for Percutaneous Image. Based devices and total facet replacement systems. Food and Drug Administration FDA through the premarket approval process.
The cost for male-to-female reassignment is 7000 to 24000 while the cost for female-to-male reassignment can exceed 50000. This surgery is rarely covered by insurers but it is covered by Medicaid in Washington. WellFirst Health Medical Policy.
Over 20000 patients have received pain relief from the Vertiflex Procedure since FDA approval. It is also covered by other commercial insurance companies. VertiFlex won reimbursement coverage from the Centers for Medicare Medicaid Services for the companys Totalis direct decompression.
Yes Medicare and Medicaid provide reimbursement coverage for Vertiflex spinal stenosis treatment. These treatments are effective in only a small percentage of patients. We are delighted by BCBS SCs positive insurance coverage policy that includes coflex.
Regulatory Status In 2015 the Superion Interspinous Spacer ISS VertiFlex now Superion Indirect Decompression System was approved by the US. It provides patients with a clinically proven minimally invasive solution that is designed to deliver long-term relief from the leg and back pain associated with LSS. Patients experience 70 relief from their back pain 80 reduction of leg pain and after 5 years over 90 of patients are still satisfied with their results.
The Vertiflex Procedure is redefining the treatment of LSS for patients. To learn more about whether the Vertiflex procedure is covered by your insurance plan contact us for more information. CMS has decided to extend.
Coding and Payment Guide for Medicare Reimbursement. A 5-year case study with 471 patients concluded. Medicare established coverage for the mild procedure earlier this year.
In the clinical study most patients on opioids stopped using them after the Vertiflex Procedure. 10 Percutaneous interspinous spacer VertiFlex requires. Percutaneous Interspinous Spacer VertiFlex 1 of 2.
It is effective in reducing leg pain by 75 at 60 months. These are not covered in this policy.