Coverage generic options and costs. XARELTO is a prescription medicine used to.
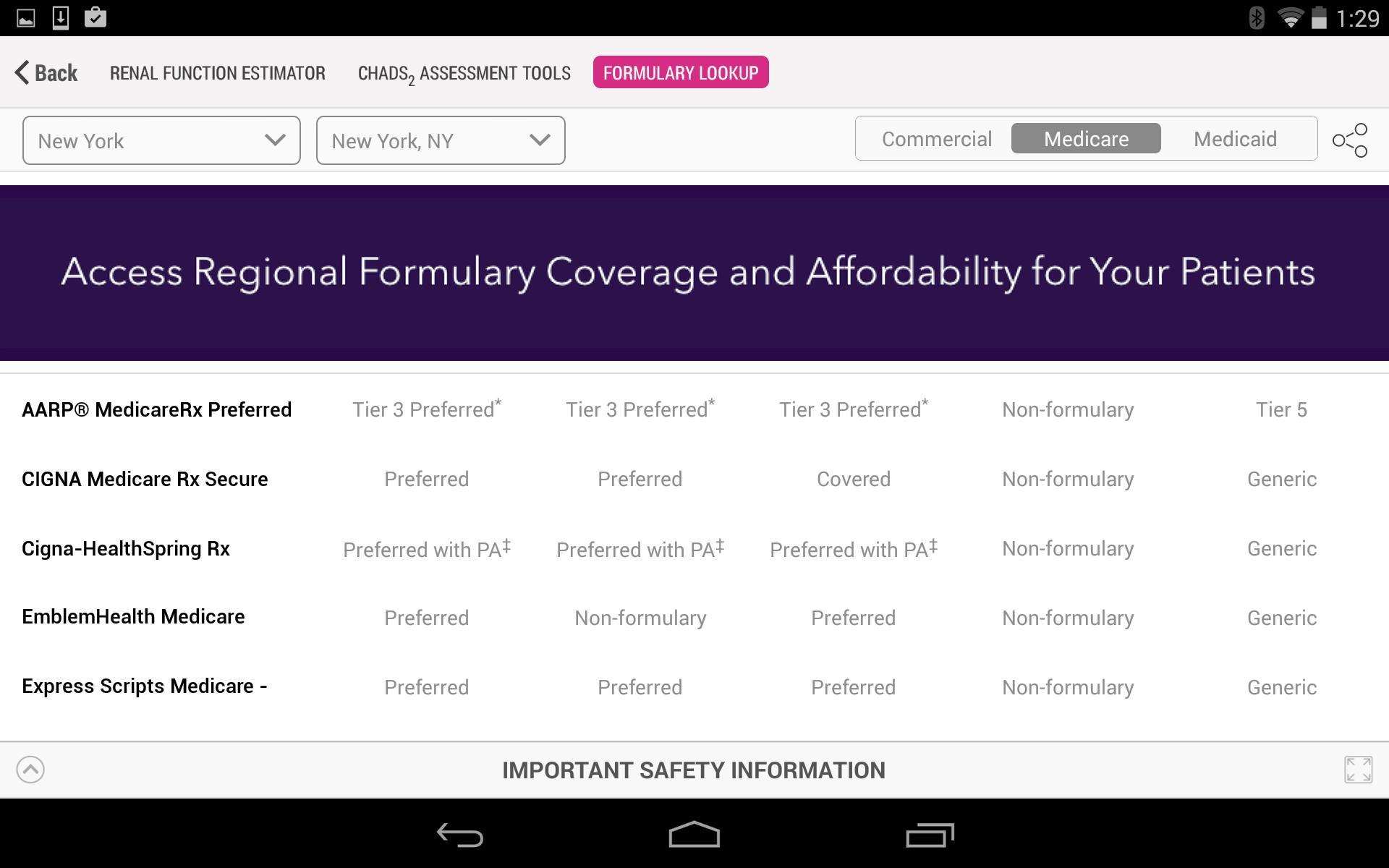 Xarelto Doccenter For Android Apk Download
Xarelto Doccenter For Android Apk Download
Most Medicare Advantage beneficiaries 88 percent are enrolled in MA-PDs.
Xarelto medicare coverage. Does Medicare cover Xarelto. Anzeige Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more. 2020 complete drug list formulary NCgov.
WHAT IS XARELTO rivaroxaban. Find affordable quality Medicare insurance plans that meet your needs. Reduce the risk of stroke and blood clots in people who have a medical condition called atrial fibrillation that is not caused by a heart valve problem.
If you are enrolled in Medicare and are using Medicare coverage to pay for your medication our Medicare Resource Guide provides information on sources for cost support that may be available. 1 Medicare Advantage plans that offer prescription drug coverage are called Medicare Advantage Prescription Drug Plans MA-PD. CODES 9 days ago Xarelto is a brand name for the drug rivaroxaban.
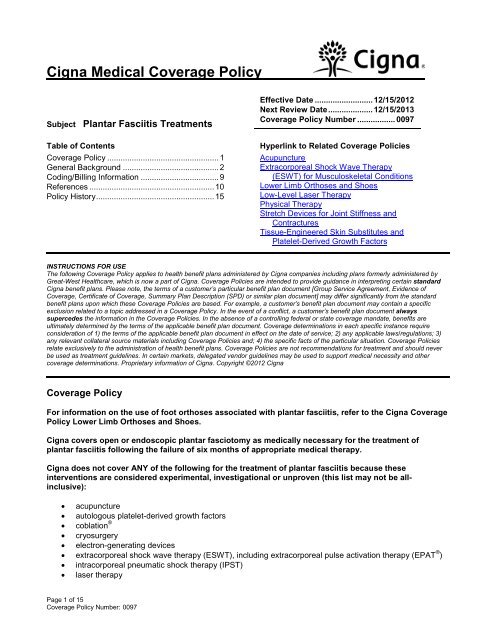
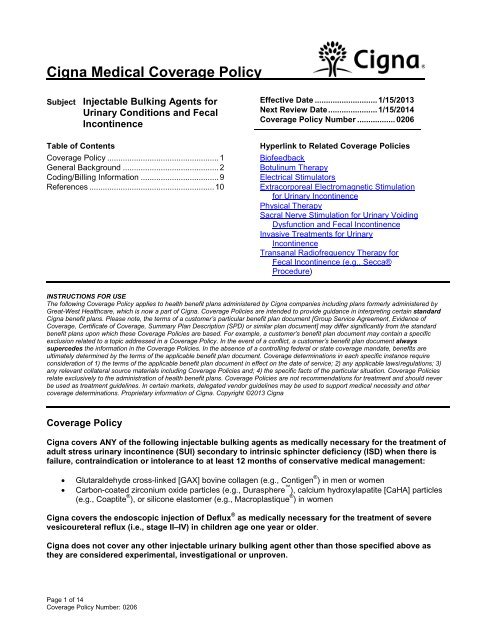
Medicare Coverage for Xarelto In order to qualify for coverage under Medicare benefits that include prescription drugs like a Medicare Advantage plan with drug coverage MA-PD or a stand-alone Part D Prescription Drug PlanPDP the medication should be considered medically necessary and approved for treatment of the targeted condition. Anzeige Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more. Reduce the risk of stroke and blood clots in people who have a medical condition called atrial fibrillation that is not caused by a heart valve problem.
The most common use is in patients with DVT. A drug list or formulary is a list of prescription drugs covered by your plan. XARELTO is a prescription medicine used to.
Does Medicare Cover Xarelto. Xarelto is a brand name for the drug rivaroxaban. Your Medicare coverage for Xarelto will depend on which part of Medicare youre using.
This percentage may not represent 100 of formulary lives due to data limitations. Can I get my drug while I wait for an exception. Xarelto is a prescription medication used to prevent blood clotting.
It is covered by most Medicare and insurance plans but some pharmacy coupons or cash prices may be lower. Youll need to be enrolled in a part of Medicare that includes prescription drug coverage. With atrial fibrillation part of the heart does not beat the way it should.
There are 2 options you may be able to consider for Medicare prescription drug coverage. Original Medicare does not typically cover prescriptions. XARELTO is a prescription medicine used to.
XARELTO and Medicare XARELTO and Medicare. 98 of Medicare Advantage plans and Medicare Part D plans cover Xarelto. Medicare is a federal program that provides health insurance coverage to the following types of people.
There are currently no generic alternatives for Xarelto. Depending on how this drug is used it may be covered by either Medicare Part B doctor. Medicare and Xarelto.
A person must be enrolled in a Medicare Part D prescription drug. Does Medicare Cover Xarelto. With atrial fibrillation part of the heart does not beat the way it should.
28 Zeilen XARELTO is indicated for the reduction in the risk of recurrence of. Medicare covers the cost of the prescription medication under certain conditions. If you receive health care coverage through Original Medicare Part A and Part B XARELTO is not covered by Medicare Part B.
1 To see the formulary coverage for your patients enter your ZIP code. XARELTO is widely accessible nationwide with preferred coverage for 95 of commercial and 95 of Medicare Part D patients. Asked May 19 2013 in.
Find affordable quality Medicare insurance plans that meet your needs. Founder Georgia Medicare Plans AtlantaGA. With atrial fibrillation part of the heart does not beat the way it should.
Parts of Medicare cover the cost of prescription medication including Part A Part D and Advantage plans. When Does Medicare Cover XARELTO. Most patients with Medicare pay between 0 and 94 per month for XARELTO.
Reduce the risk of stroke and blood clots in people who have a medical condition called atrial fibrillation that is not caused by a heart valve problem. 34 This number represents Medicare Part D including those with LIS. Your results will appear below.
Individuals over age 65 with a work history Individuals with certain disabilities who have been disabled for at least 2 years Individuals diagnosed with end-stage renal disease ESRD.