UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Helpful Guide to completing the Application.
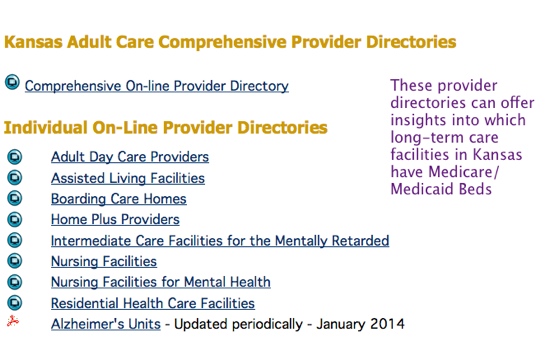 How To Identify Kansas Medicaid Facilities
How To Identify Kansas Medicaid Facilities
This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original.
Kansas medicare medicaid. Centers for Medicare and Medicaid Services 601 East 12th Street Suite 235 Kansas City MO 64104. Medicaid is administered by the Kansas Department of Health and the Environment. When a state wants to change any of the Medicaid benefits it offers or change the way in which they are offered it must submit a State Plan Amendment SPA.
These counselors are affiliated with Senior Health Insurance Counseling for Kansas a service of the Kansas Department on Aging. A federal government website managed and paid for by the US. According to information provided by the state KanCare is a statewide Medicaid reform effort that expands managed care to almost all Medicaid state plan populations including some dual eligibles for physical behavioral and long term services and supports.
Kansas Medicaid also referred to as the Kansas Medical Assistance Program KMAP is a jointly-funded state and Federal government program that pays for medically necessary services. Program of All-Inclusive Care for the Elderly PACE. Senior Health Insurance Counseling for Kansas SHICK Kansas Senior Medicare Patrol SMP Medicare Improvements for Patients and Providers Act MIPPA Alzheimers Disease Task Force.
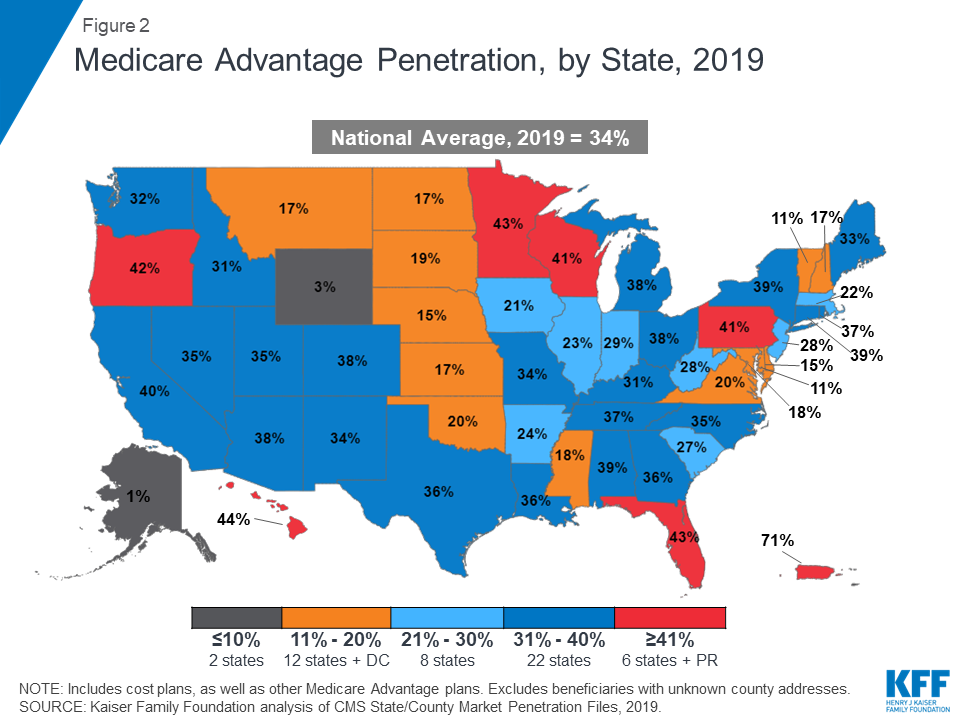
CMS recently established an electronic submission process. As of mid-2020 27 percent of Medicare beneficiaries in Kansas 116505 people were enrolled in private plans obtained through Medicare Advantage insurers this does not count people with Original Medicare who supplement their coverage with private Medigap or Medicare Part D coverage. KanCare is the program through which the State of Kansas administers Medicaid.
Client Assessment Referral and Evaluation CARE Spousal Impoverishment Law. The KanCare program is the State of Kansas managed care program. Centers for Medicare and Medicaid Services CMS for the Kansas Modular Medicaid System KMMS Stage 1.
DXC has implemented and attained certification from the US. The KanCare program went into effect Jan. 7500 Security Boulevard Baltimore MD 21244.
Josh Schultz has a strong background in Medicare and the Affordable Care Act. You can request an application for Medicaid ABD or an MSP by calling call 800-792-4884. Enrollment in the plan depends on the plans contract renewal with Medicare.
KC-1501 ED Application Guide. To qualify for Medicare you must be either a United States citizen or a legal permanent resident of at least five continuous years. Calling Medicare at 1-800-633-4227 1-800-MEDICARE Calling 1-800-860-5260 to schedule a free confidential counseling session with a trained counselor.
Medicaid pays for medical services for children and their. The process of applying for Medicare in Kansas is the same as in any other state. For reference private Medicare enrollment had climbed to 40.
Aetna Better Health of Kansas 855-221-5656. The Kansas Medicaid program which is called KanCare has not been expanded under the ACA. To request and application call.
The KanCare health plans are Aetna Better Health of Kansas. To apply online visit the Medical Consumer Self-Service portal. This website contains more information about applying for Medicaid in Kansas.
KanCare is provided to all Medicaid and CHIP consumers. KanCare also provides managed care authority for the states concurrent section 1915c home and. Once the CMS Regional Office receives a SPA.
These counts do not include the Consumer Assessment of Healthcare Providers and Systems CAHPS Health Plan Survey 50H Adult Version Medicaid CPA-AD measure which is publicly reported by CMS but uses a different summary statistic. The KanCare program began in January 2013. 05 2019 The Kansas Department of Health and Environment KDHE in collaboration with DXC Technology NYSE.
A bipartisan compromise to expand coverage was proposed in 2020 but the legislation was derailed due to unrelated abortion legislation and did. KanCare offers 3 health plans to coordinate healthcare for their Medicaid beneficiaries. Centers for Medicare Medicaid Services.
TYSONS Va Dec. When a state did not report a measure or used non-Core Set specifications the measure is not included below or in the. Kansas has contracted with three health plans or managed care organizations MCOs to coordinate health care for nearly all beneficiaries.
Launched in January 2013 KanCare is delivering whole-person integrated care to more than 415000 people across the state. 1 2013 and replaced the Kansas Medicaid Program.